Insulin ranks as one of the great discoveries of the Twentieth Century. Initially, it was thought of primarily in terms of providing an explanation and a solution to diabetes. Subsequent research reduced expectations that insulin was a “cure” to diabetes, yet broadened the range of conditions in which insulin appeared to be active. Similarly, organs beyond the pancreas became recognized as being linked to insulin’s activities. These included the muscles as repositories for glucose disposal after meals and even the bones as regulators of insulin’s actions. The concept of insulin resistance, meaning poor responses to insulin’s actions in peripheral tissues, emerged as a major explanation for a variety of conditions under the headings Syndrome X and metabolic syndrome. Just as insulin resistance is a major component in the course of diabetes type 2, it also now is linked to many other conditions.
Commonly over the long term in type 2 diabetes mellitus, insulin resistances increases blood glucose levels followed by a compensatory rise in circulating insulin concentrations with the latter being the body’s attempt to adapt to the former. Consequences include high blood sugar levels, prolonged high insulin levels, the appearance of medical complications and the exhaustion of the pancreas’ ability to produce insulin.
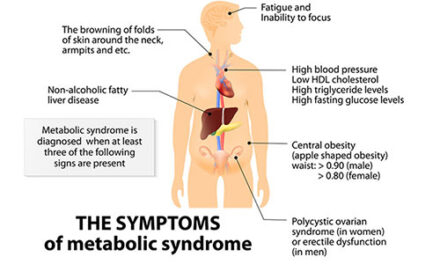
The core of the metabolic syndrome thus is the dysregulation and dysfunction involving glucose and insulin. Aside from these, secondary characteristics encompass central obesity, hypertension, and dyslipidemias—especially hypertriglyceridemia and low levels of HDL cholesterol. In addition to participating in the development of many facets of the metabolic syndrome, impairment in insulin sensitivity also appears to be involved in the aging process by promoting inflammation, endothelial dysfunction, the production of advanced glycation end products (AGE), and oxidative stress. Downstream consequences of these dysfunctions include cardiovascular disease and cancer.
Several major questions have emerged regarding the appearance of the metabolic syndrome. Western medicine, unlike, for instance, traditional Chinese and Indian medicine, tends to pursue and treat the various arms of the metabolic syndrome as distinct clinical entities. Much of the research on the syndrome within allopathic medicine over the past three decades has been aimed at arguing against this separation. Another issue is the level of insulin resistance that should be taken as requiring attention. Most clinicians consider a level of circulating glucose under fasting conditions in the range of 100–125 mg/dl to be pre-diabetic. And then there is the issue of inevitability, which is to say, does the metabolic syndrome arise as a consequence of aging?
Early Signs of the Metabolic Syndrome in Non-Diabetics
For some time, there have been questions as to what should be acceptable as a normal fasting glucose level. Circulating glucose within levels generally accepted as normal can influence brain function in an unfavorable manner and increasing hemoglobin AlC (HbAlC) and insulin levels even in the non-diabetic range may affect blood pressure adversely. Such observations lead to suspicions that minor insulin resistance predicts the early onset of many disturbed health parameters involved in the metabolic syndrome. Recently Harry G. Preuss and co-authors, of whom I am one, addressed just such questions in “Fasting Circulating Glucose Levels in the Non-Diabetic Range Correlate Appropriately with Many Components of the Metabolic Syndrome.” 1 Those with special interests should consult that journal and a forthcoming more detailed article.
To be sure, despite access to a large number of medical records, our study faced technical limitations. Because we worked exclusively with subjects possessing non-diabetic fasting glucose concentrations, the other measured clinical values, for the most part, fell in the accepted normal range. Therefore, correlations rather than exact numbers were largely used to determine alterations in health modalities. For corroboration, however, we examined statistical differences in the various parameters between the highest and lowest quartiles associated with these fasting glucose levels. Our data in this preliminary study are representative of the general population in middle and late middle age. The hypothesis is that glucose/insulin perturbations are at the heart of the increased incidence and severity of the various constituents making up the metabolic syndrome and could hasten/ worsen the aging process. A major goal in the study was to cast light on the issue of whether aging itself is associated with the development of the components of the metabolic syndrome or whether, to the contrary, containment of fasting insulin/glucose levels to a relatively low level reduced the appearance of the metabolic syndrome components despite advancing age.
Findings
Despite the fact that the population sample consisted entirely of individuals with fasting blood glucose readings below those of diabetes, there was a clear positive correlation between rising glucose levels and metabolic syndrome components. As expected, the average, baseline values of most parameters were in the accepted normal range. Nevertheless all of the following increased more or less in tandem with rising glucose levels: body weight, body fat mass, systolic/diastolic BP, HbA1C, circulating levels of insulin, triglycerides, hsCRP (highly sensitive C-reactive protein) and along with a number of other components representing inflammation and liver health. Elevated non-diabetic glucose levels were associated with signs of augmented inflammation (increased hsCRP, white cell and neutrophil cell counts) and liver perturbations (increased ALT) proposed to play a role in the metabolic syndrome.
On the reverse side, high-density lipoprotein (HDL) showed a negative correlation, meaning that higher blood glucose levels lead to lower HDL levels. Put another way, unlike fasting glucose, when total cholesterol became the independent variable, the majority of these health parameters improved showing beneficial correlations compared to fasting glucose. However, when examining the total cholesterol minus HDL-cholesterol correlations, all benefits of total cholesterol are lost, suggesting that the benefits noted with total cholesterol are primarily due to the presence of HDL-cholesterol.
We concluded that the early onset of the various risk factors correlating with circulating fasting glucose suggests a significant role for insulin resistance in the development of the metabolic syndrome. HbA1C and insulin values are also be linked to insulin resistance, but we chose to follow a more common, clinically available marker—circulating fasting glucose levels. Fasting glucose concentrations and the levels of HbA1C and insulin are significantly correlated, therefore findings are similar whether one tests using fasting glucose levels or insulin levels.
What is the ideal range of fasting blood glucose? Based on our preliminary study, the health data were significantly better with glucose levels in the range of 67–86 mg/dL than at 98–125 mg/dL. Across a wide range of variables, lower definitely was better. Another finding, one only touched on in the provisional version of the study described here, is that aside from blood pressure, age did not seem to play a significant independent role in determining metabolic syndrome health risks and even with regard to increasing systolic blood pressure (the top figure) the influence was less than expected. Glucose and insulin levels were the primary drivers of risk factors, not age.
Conclusion
If glucose and insulin levels are the primary sources of metabolic syndrome risks, then enhancing insulin sensitivity and lowering circulating glucose levels are steps that should be taken to promote and maintain health. Fortunately, many of the means to encourage better glucose control are relatively easy. Diet no doubt is key. Sugar, refined carbohydrates and excessive calorie consumption definitely are not friends of good health. Neither are bad eating habits, which include skipping breakfast, eating late in the day and snacking, especially at bedtime. Exercise can be very helpful, particularly taking at least a 15-minute brisk walk before lunch and again later in the day. All of these measures amount to the ounce of prevention advice that actually does work, but only so long as it is followed!
References:
- Preuss, H. G., Clouatre, D, et al. Fasting Circulating Glucose Levels in the Non-Diabetic Range Correlate
- Appropriately with Many Components of the Metabolic Syndrome. The Original Internist June 1, 2016, pp. 78ff.